Research has shown that there are huge benefits of using continuous glucose monitoring (CGM) in people with diabetes, particularly for those with type 1 diabetes.
Whether you use CGM in combination with multiple daily injections (MDI) or with an insulin pump, if you use CGM regularly you can improve your day-to-day blood glucose levels (BGLs), your HbA1c (the 3-month average test for diabetes), reduce the risk of developing diabetes related complications and hypoglycaemia, all through monitoring your Time in Range.
What is Time in Range?
The Time in Range (TIR) is the percentage of time you spend with your sensor glucose (SG) levels in a particular target range. TIR can also be reflected as the hours per day spent in range. Time in Range includes three key CGM measurements:
1. TIR, which is the percentage of readings and time per day within the target glucose range
2. Time Below Range (TBR), which is the time spent below the target glucose range
3. Time Above Range (TAR), which is the time spent above target glucose range
The main goal is to increase the TIR whilst avoiding hypoglycaemia, or in other words, reducing the TBR.
What is the optimal Time in Range target?
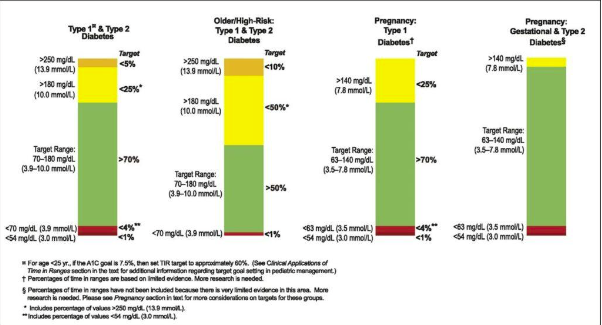
Most diabetes experts agree that a SG target range of 3.9-10.0 mmol/L is ideal. However special considerations, such as pregnancy or other health conditions, will need to be taken into account. Talk to your diabetes healthcare professional about what your personal target range should be.
For most people with diabetes it is recommended:
- To spend at least 70% of the day TIR (3.9-10.0 mmol/L)
- To spend less than 4% of the day in TBR (under 3.9 mmol/L)
- And less than 1% of the day under 3.0 mmol/L
- And, as a result, to spend less time in TAR (above 10.0 mmol/L)
Hypoglycaemia is an acute complication of diabetes and hence it is also important to look at both the time in range as well as the time below range.
Higher percentages of TIR, like lower HbA1c results, are associated with a decreased risk of the development of diabetes related complications.
How is TIR different from HbA1c?
Having said that, research shows that a TIR of 70% in most cases corresponds with a HbA1c of 7% (53 mmol/mol), whereas a TIR of 50% is correlated to a HbA1c of 8% (64 mmol/mol).
Similarly, an increase of TIR of 10% (which is equivalent to 2.4 hours per day more time spend in range) corresponds to a decrease in HbA1c of around 0.5% (5.0 mmol/mol). So, there is certainly a link between the 2 measures.

So why not stick with HbA1c, like we are used to?
In short, because HbA1c does not give any indication as to how much time you spent in hypoglycaemia. Let me clarify this statement with an example:
You can have a HbA1c of 7.0% with blood glucose levels between 4.0 and 8.0 mmol/L, but you can also have a HbA1c of 7.0% with BGLs between say 2.0 and 22.0 mmol/L.
Also, some medical conditions can affect the HbA1c measure, including conditions such as haemoglobinopathies (a range of conditions that affect haemoglobin), anaemia, iron deficiency and pregnancy.
And, HbA1c is a “weighted average of glucose levels”; this means that glucose levels in the past 30 days contribute considerably more to the level of HbA1c than do glucose levels from 90-120 days earlier. If you had big changes in your BGLs in the last month (such as often happens with special occasions or during holidays such as Christmas or Easter) this may have a significant impact on your HbA1c.

.
Limitations of only using TIR
CGM lets you observe changes in your glucose levels and daily profiles, including patterns of hypo- or hyperglycaemia and this can greatly assist you (and your diabetes healthcare professional) in making therapy decisions and any lifestyle changes.
However, when glucose levels are changing rapidly there may be a delay in the CGM registering the SG changes. This is also known as lag time (more on this later).
Also, CGM is not a “set and forget” system; it requires you (and your diabetes healthcare professional) to interpret the data and act upon this appropriately. You would need to actively use CGM for it to be effective and this can be costly.

How can I improve my TIR?
First, address any hypos you may be having. By avoiding hypoglycaemia, you will be able to reduce your TBR and often you will minimise rebound hyperglycaemia at the same time, which will reduce your TAR and hence improve your TIR. Talk to your diabetes healthcare professional for advice on how you can achieve this.
People with type 2 diabetes tend to have less variability in their glucose levels and tend to have less hypoglycaemia than those with type 1 diabetes, therefore people with type 2 diabetes can often achieve more TIR, more easily.
You can improve your TIR by counting carbohydrates actively and accurately, by adjusting your bolus (pre-meal) insulin doses based on your current SG or BG level, your glucose target, your insulin to carbohydrate ratio (ICR), insulin sensitivity factor (ISF), any insulin left on board (IOB) and your insulin action/duration.
When it comes to making insulin dose adjustments; slow and steady wins the race.
Physical activity and meal composition (the balance between carbohydrates, protein, fat, vitamins, minerals and fibre) of course also play a major role and need to be considered. When making changes to your insulin regimen, always follow the advice of your diabetes healthcare professional.

.
References:
1. Andrade Lima Gabbay et al, Diabetology & Metabolic Syndrome, published 16 March 2020; Time in range: a new parameter to evaluate blood glucose control in patients with diabetes. https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-020-00529-z
2. Battelino et al, Diabetes Care, August 2019; Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. https://care.diabetesjournals.org/content/42/8/1593
3. R. W. Becket al, J Diabetes Sci Technol. 13 January 2019; The relationships between time in range, hyperglycemia metrics, and HbA1c. https://pubmed.ncbi.nlm.nih.gov/30636519/
4. R. A. Vigersky, C. McMahon, Diabetes Technology & Therapeutics, online 1 February 2019; The Relationship of Hemoglobin A1C to Time-in-Range
in Patients with Diabetes. https://www.liebertpub.com/doi/full/10.1089/dia.2018.0310
5. T. Danne et al, Diabetes Care December 2017; International Consensus on Use of Continuous Glucose Monitoring. https://care.diabetesjournals.org/content/40/12/1631